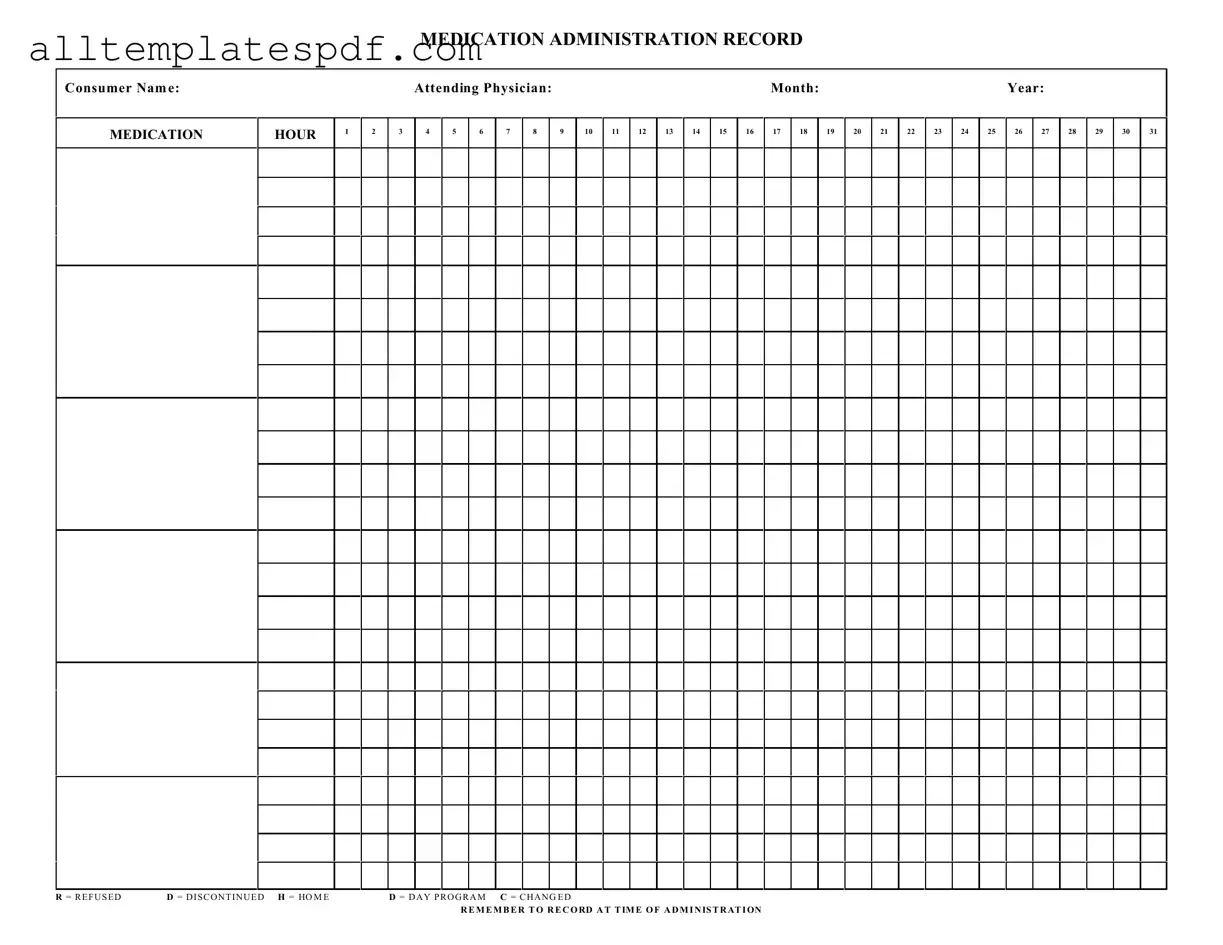
Fill Out a Valid Medication Administration Record Sheet Form
The Medication Administration Record Sheet is an essential tool used in healthcare settings to document the administration of medications to patients. This form helps ensure that medications are given at the correct times and allows healthcare providers to track any changes or refusals. To effectively manage medication administration, be sure to fill out the form by clicking the button below.
Open Editor
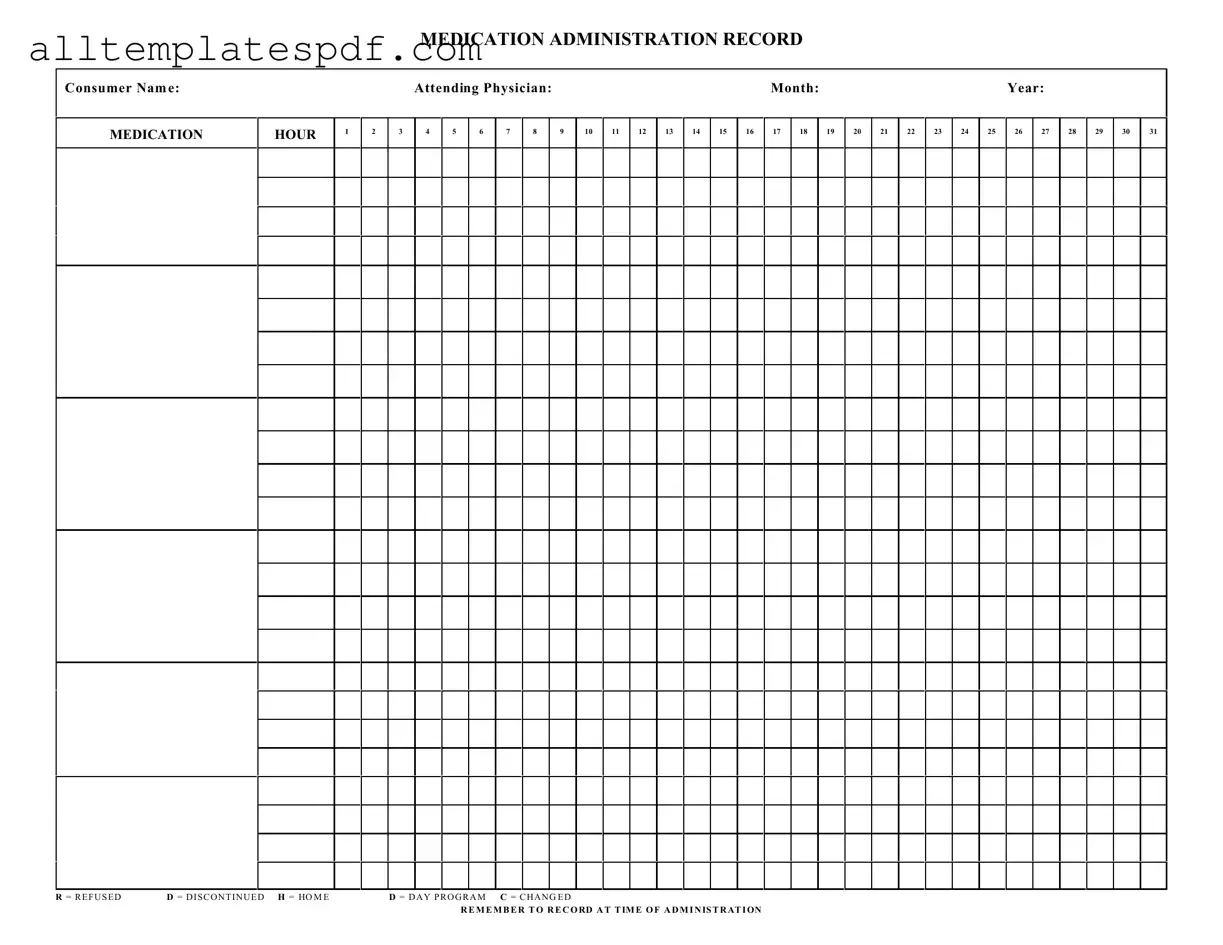
Fill Out a Valid Medication Administration Record Sheet Form
Open Editor
Fast and easy form completion
Complete Medication Administration Record Sheet digitally — fast and easy.
Open Editor
or
↓ Medication Administration Record Sheet PDF Form