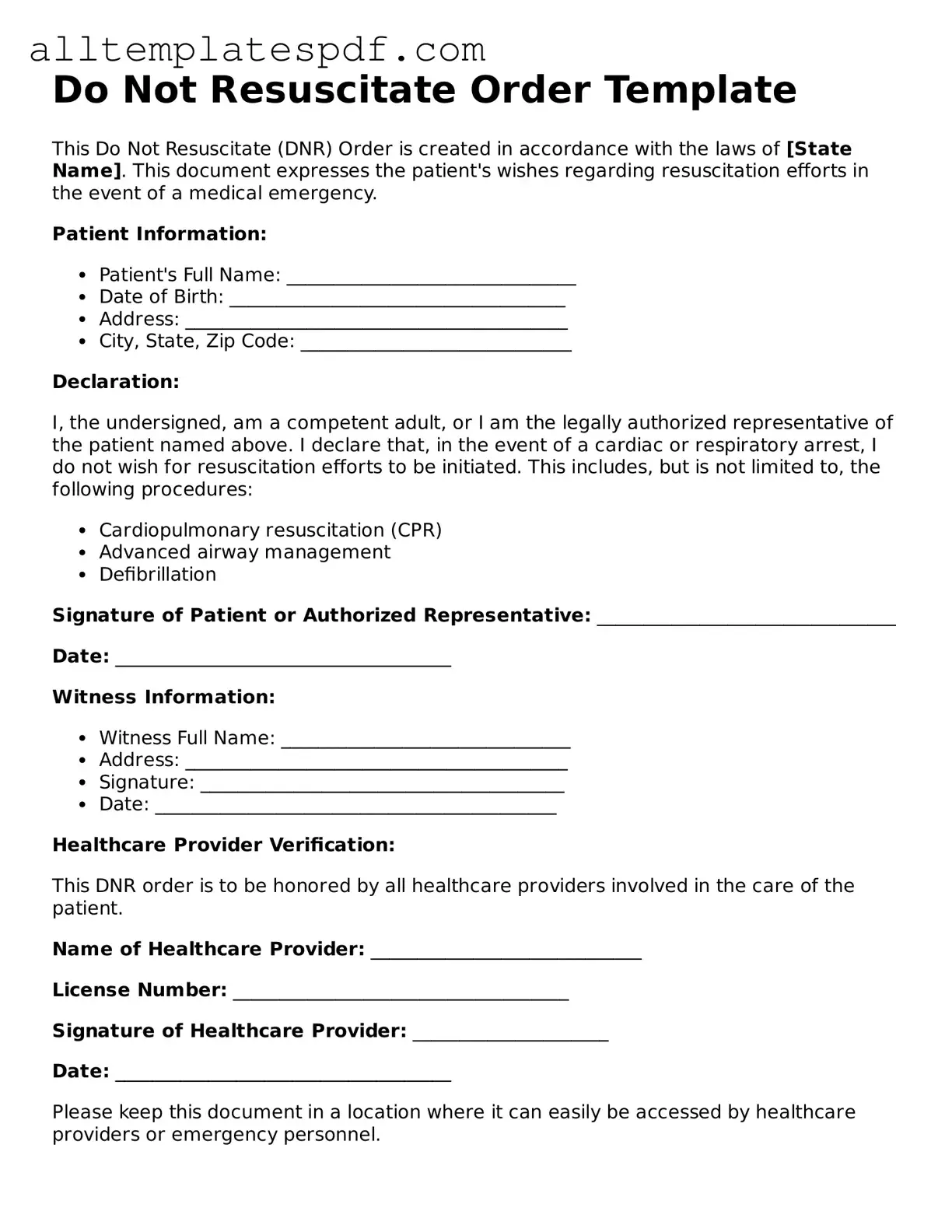
Attorney-Approved Do Not Resuscitate Order Template
A Do Not Resuscitate (DNR) Order is a legal document that instructs medical personnel not to perform cardiopulmonary resuscitation (CPR) if a person's heart stops beating or they stop breathing. This form is crucial for individuals who wish to forgo life-saving measures in certain medical situations. To ensure your wishes are respected, consider filling out the DNR Order form by clicking the button below.
Open Editor
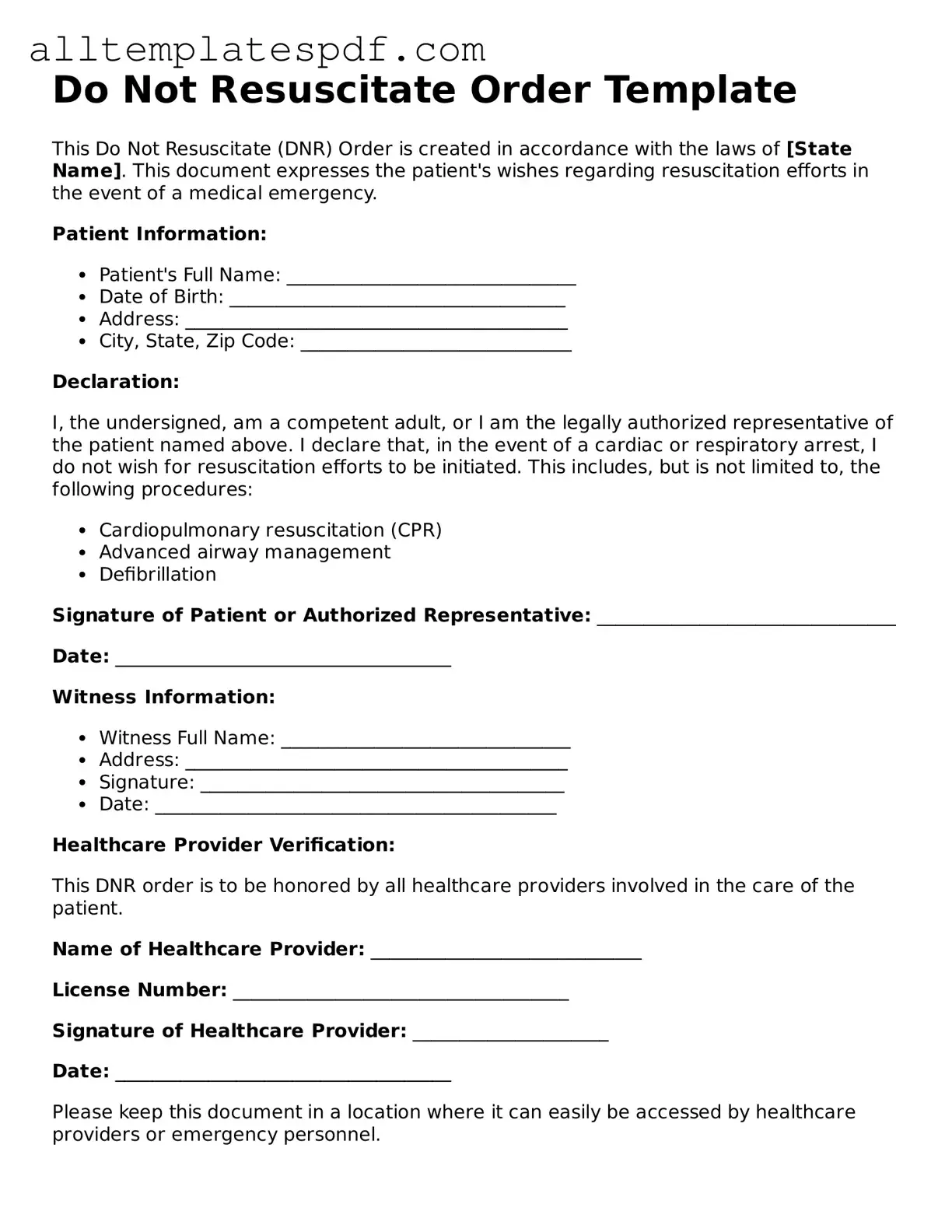
Attorney-Approved Do Not Resuscitate Order Template
Open Editor
Fast and easy form completion
Complete Do Not Resuscitate Order digitally — fast and easy.
Open Editor
or
↓ Do Not Resuscitate Order PDF Form