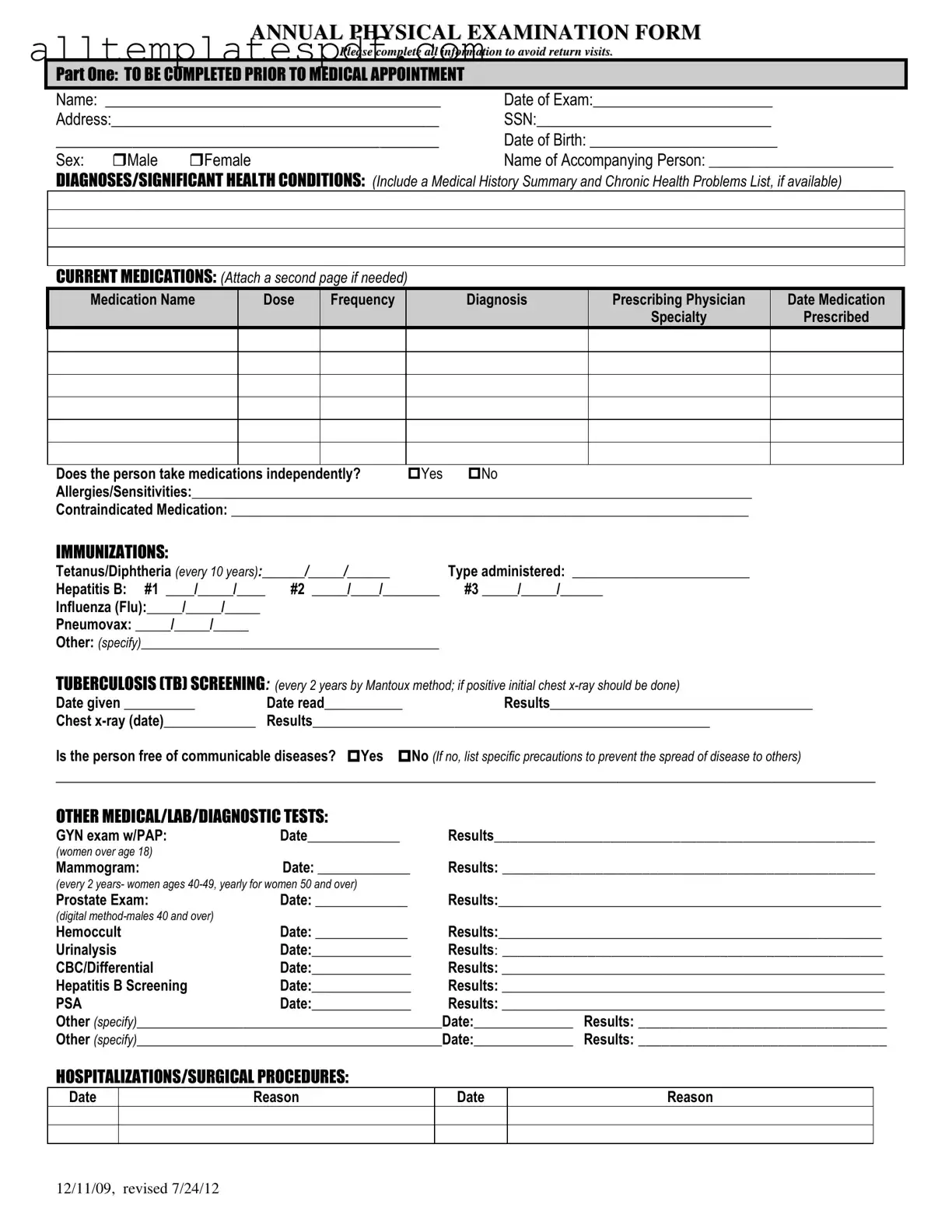
Fill Out a Valid Annual Physical Examination Form
The Annual Physical Examination Form is a crucial document designed to collect comprehensive health information before your medical appointment. It helps ensure that your healthcare provider has all the necessary details to deliver the best care possible. Completing this form accurately can prevent unnecessary return visits, so please take a moment to fill it out by clicking the button below.
Open Editor
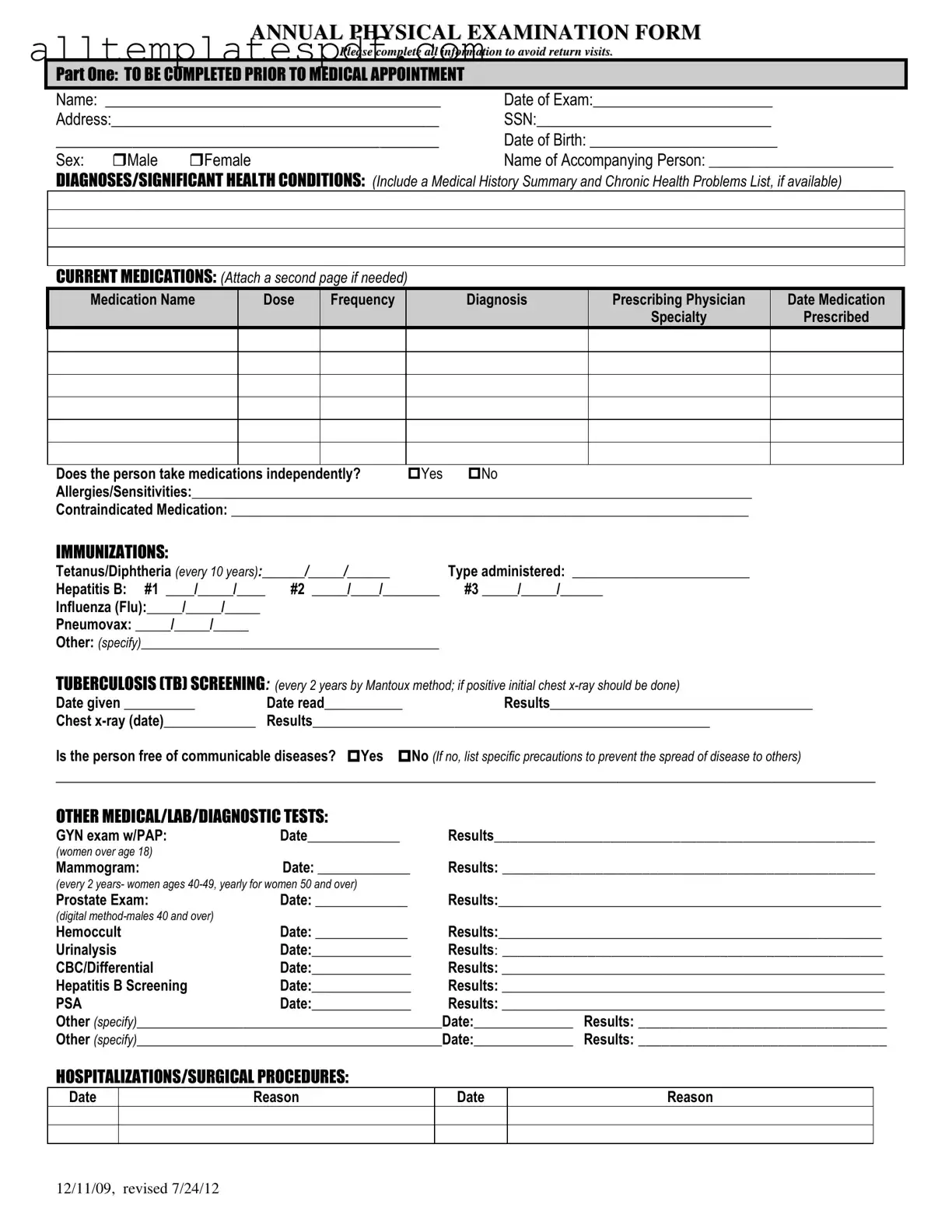
Fill Out a Valid Annual Physical Examination Form
Open Editor
Fast and easy form completion
Complete Annual Physical Examination digitally — fast and easy.
Open Editor
or
↓ Annual Physical Examination PDF Form