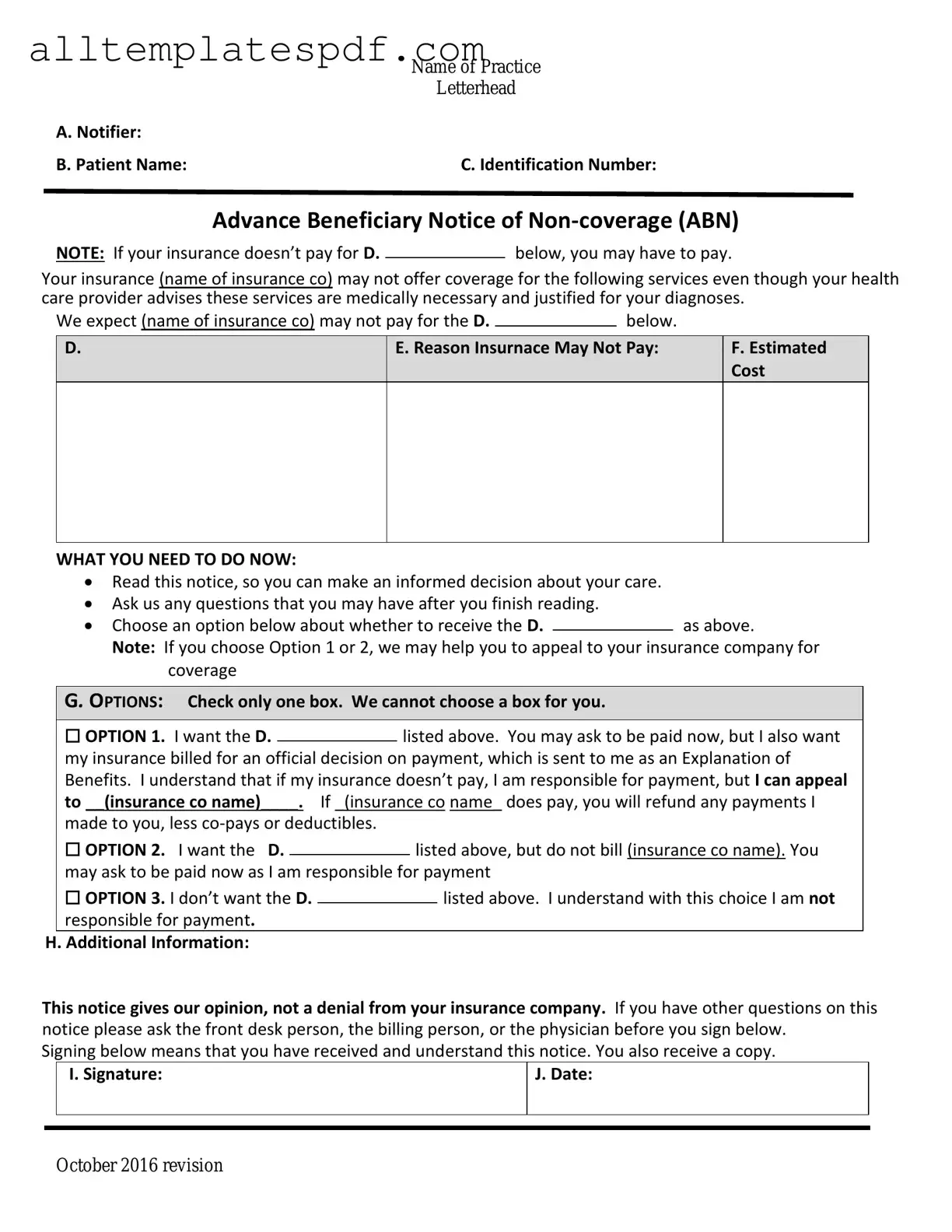
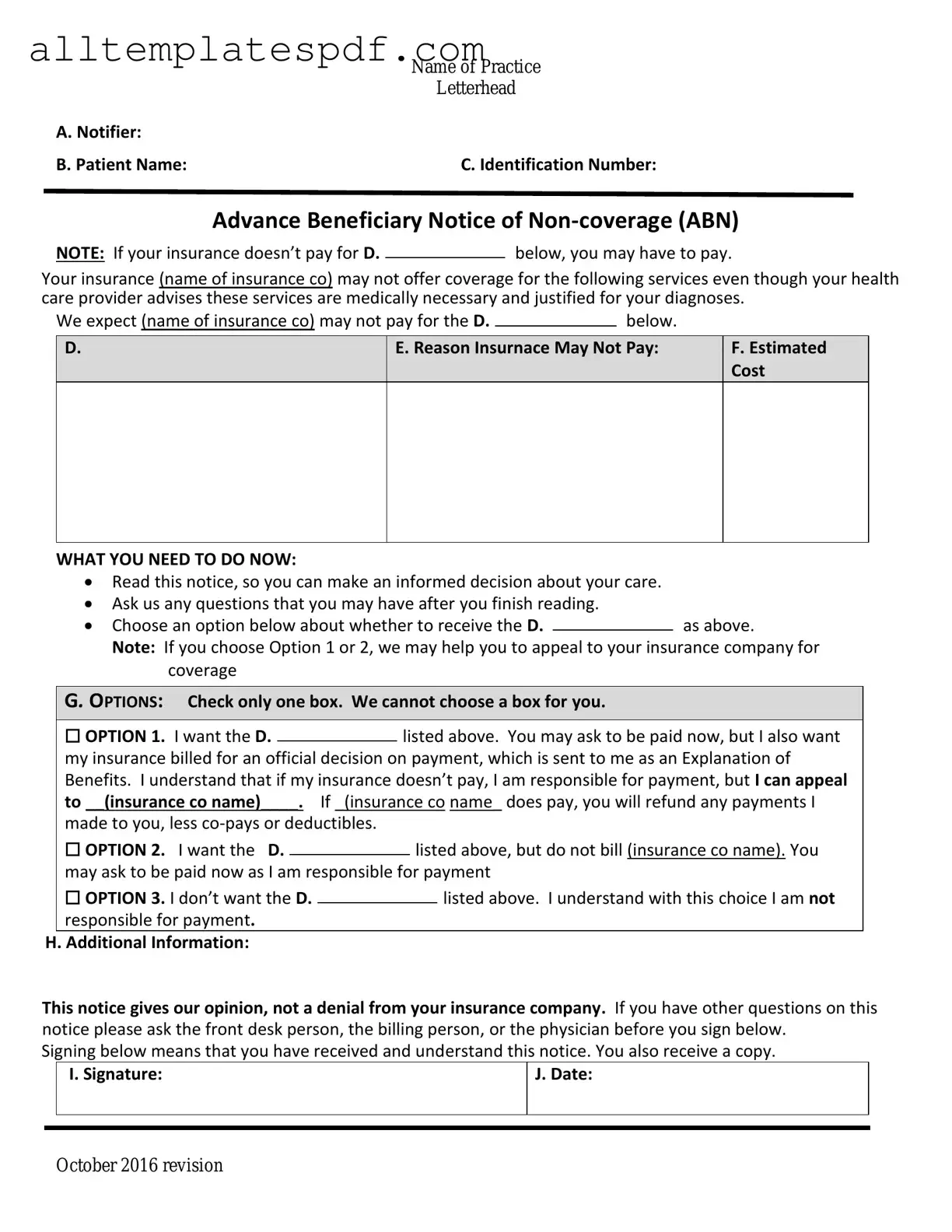
Filling out the Advance Beneficiary Notice of Non-coverage (ABN) form can be a straightforward process, but many individuals make common mistakes that can lead to confusion and complications. One prevalent error is failing to provide complete information. When a beneficiary does not fill in all required fields, it can delay the processing of their claim.
Another frequent mistake is not understanding the purpose of the ABN. This form is meant to inform beneficiaries that Medicare may not cover a service. If individuals do not grasp this concept, they may mistakenly assume that all services listed will be covered, leading to unexpected out-of-pocket costs.
Additionally, beneficiaries often neglect to sign and date the form. A signature is crucial as it indicates that the beneficiary acknowledges the potential for non-coverage. Without a signature, the form may be considered invalid, complicating the claims process.
Some individuals also misinterpret the options provided on the form. The ABN typically presents choices regarding whether to receive the service or not. Misunderstanding these options can result in beneficiaries either opting for services they do not want or declining necessary care.
Another common issue arises from not keeping a copy of the completed ABN. Beneficiaries should always retain a copy for their records. This can be essential if questions about coverage arise later.
Moreover, beneficiaries sometimes fail to ask questions when they do not understand the form. It is vital to seek clarification from healthcare providers if there is any uncertainty. Ignoring this step can lead to serious misunderstandings regarding coverage.
In some cases, individuals may not be aware of the time-sensitive nature of the ABN. It must be filled out and submitted promptly to avoid delays in receiving services. Delays can lead to missed appointments or treatments, which can adversely affect health outcomes.
Another mistake is overlooking the importance of reviewing the details of the services listed on the ABN. Beneficiaries should ensure that the services they are signing for are accurate. If there are discrepancies, they must address them immediately.
Lastly, beneficiaries sometimes assume that the ABN is the only form they need to fill out. In reality, there may be additional paperwork required for certain services or procedures. Failing to complete all necessary documentation can result in further complications down the line.